Breaking Through The Blood–Brain Barrier: The Rise Of Focused Ultrasound
By Neal F. Kassell, MD, founder and chairman, Focused Ultrasound Foundation
Innovative medicines are delivering remarkable results for patients. CAR-T therapies can send cancer into remission; gene therapies can reverse devastating conditions; and antivirals can render the virus that causes AIDS undetectable. Despite the tantalizing success of many therapeutics, some diseases continue to be difficult adversaries, and not all patients benefit from treatment.
Consider immunotherapies based on immune checkpoint inhibition. These drugs have become an important pillar for the management of cancer, yet response rates remain frustratingly low. One study estimated that less than 15% of cancer patients respond, with just a handful of tumor types being particularly susceptible, including non-small cell lung carcinoma, renal cell carcinoma, and melanoma.1
Another well-publicized source of frustration in the biopharmaceutical industry is the staggering 98% failure rate of drug candidates for Alzheimer’s disease. The complexity of the disease has proven to be vexing, as well as the roadblock created by the blood–brain barrier (BBB). The BBB is a network of tightly connected endothelial cells that line capillaries in the brain, protecting it from blood-borne incursions but also limiting the ability of therapeutics to reach their targets.
Novel strategies are needed to expand the reach of powerful immune checkpoint inhibitors and overcome the unique challenges presented by diseases that affect the brain. Focused ultrasound technology is one strategy that is revolutionizing the treatment of many conditions and has entered the fight against formidable foes like cancer and neurodegenerative diseases.
Leveraging The Power Of Ultrasound
Focused ultrasound is a noninvasive technology that is transforming the treatment of many medical disorders by targeting ultrasonic energy at tissue deep in the body without incisions or radiation. It has been approved by the U.S. FDA for nine indications to date, including essential tremor, Parkinson’s disease, prostate cancer, uterine fibroids, and pain from bone metastases. Around the world, it has been approved for use in more than 30 indications and is in various stages of research and development for 180 conditions.
Focused ultrasound brings together powerful technologies – magnetic resonance or ultrasound imaging targets ultrasound energy at the tissue to be treated, guide and control the treatment in real-time, and confirm the effectiveness of the treatment. The fundamental principle of focused ultrasound is analogous to using a magnifying glass to focus beams of sunlight on a single point to burn a hole in a leaf. With focused ultrasound, an acoustic lens is used to concentrate multiple intersecting beams of ultrasound on a target deep in the body with extreme precision and accuracy. Depending on the design of the lens and the ultrasound parameters, the target can be as small as 1×1.5 mm or as large as 10x16 mm in diameter. Where each of the individual beams passes through the tissue, there is no effect. At the focal point, however, the convergence of the multiple beams of focused ultrasound energy results in many important biological effects, creating the possibility of treating a variety of medical disorders.
Engaging In The War On Cancer
Focused ultrasound can interact with the cancer immunity cycle in many ways and is being applied to multiple tumor types in preclinical and clinical trials, with a goal of improving patient outcomes. It can be used to target many locations in the body and can modulate the immune system and facilitate drug and immune cell delivery to the tumor.2
Two translational approaches have emerged. The first involves targeting cancers that respond poorly to existing immunotherapies and/or are immunologically cold (breast, ovary, prostate, pancreas, and primary brain tumors). This approach leans heavily on data demonstrating that focused ultrasound can trigger and/or modulate an anti-tumor immune response and could offer lifesaving treatment for patients that respond favorably. An alternate approach targets diseases where focused ultrasound may provide an incremental improvement. These applications involve cancers that do respond to immunotherapies and focus on improving the efficacy of existing treatments by acting as an immune adjuvant and/or by enhancing the delivery of the immunotherapy. Positioning focused ultrasound as a drug delivery platform for approved therapies may allow integration earlier in disease progression, providing a better metric of focused ultrasound’s potential as a frontline therapy.
Focused ultrasound can be used in several modes, ranging from irreversible thermal or mechanical ablation to transient thermal or mechanical effects. Each of these modes interacts with tumor tissue in diverse ways and therefore may illicit varying immune responses. Within the body, histotripsy (non-thermal ablation), thermal ablation, and hyperthermia have been evaluated for their effects on the immune system. Histotripsy can trigger the release of damage-associated molecular patterns (DAMPs), alter cytokine and chemokine profiles, and decrease populations of pro-tumor immune cells. Histotripsy may also improve local immune cell infiltration, particularly in fibrous tumors, by disrupting the extracellular matrix. Thermal treatments can result in changes in vascular permeability and/or perfusion, production of heat shock proteins and other proinflammatory cytokines and chemokines, and an increase in cytotoxic activity from natural killer (NK) and CD8+ T cells. Immune responses, and particularly immune cell infiltration, may be improved by using a partial ablation strategy during thermal ablation.
As an example of how focused ultrasound can potentially be used in the fight against cancer, a team at the University of Virginia has treated advanced-stage breast cancer with a combination of the technology and immunotherapy to increase tumor immunogenicity. Focused ultrasound can induce immune responses in most tumors but is not enough on its own to be curative, while the immune checkpoint inhibitor pembrolizumab can induce an immune response to some types of breast cancers. The UVA team tested whether the combination of focused ultrasound ablation and pembrolizumab enhanced efficacy. Ablation causes acute thermal cellular injury and can initiate a brisk local immune response with CD8+ T cells trafficking to and infiltrating the damaged area around the tumor. In a Phase 1 clinical trial, the primary objective was to assess the adverse event profile in patients with metastatic breast cancer and determine whether the addition of pembrolizumab to focused ultrasound increases the proportion of CD8+ tumor infiltrating lymphocytes in relation to FoxP3+ regulatory T cells in the primary and pre-ablation zone. Seven days post-treatment, immune cell infiltration analysis found that CD8+ T cell counts remained the same but FoxP3+ cells decreased, suggesting that the tumor microenvironment became more immunogenic.
Moving Drugs Beyond The BBB
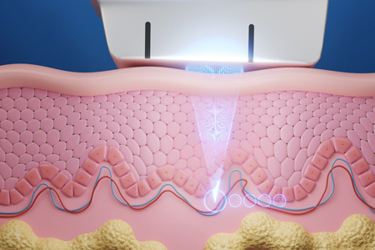
Researchers and clinicians worldwide are leveraging focused ultrasound to noninvasively, safely, and reversibly open the BBB, overcoming a major obstacle for therapies targeting neurodegenerative diseases. The mechanical effects of focused ultrasound, namely cavitation, are thought to be the principal cause of BBB disruption. Small bubbles used as a contrast agent during ultrasound imaging procedures are injected into the bloodstream during the focused ultrasound procedure. When ultrasound waves are aimed at specific parts of the brain, the bubbles expand and contract, pushing apart the tightly packed cells of the BBB. These microbubbles oscillate in the vessels and put pressure on the endothelium, forcing apart the tight junctions. Normally, only small molecules (typically smaller than 400 Da) with the proper charge and hydrophilicity can cross the BBB, but disruption of this barrier with focused ultrasound has been shown to enable molecules as large as 150 kDa to cross.
Lipsman et al. were the first to report the use of focused ultrasound plus microbubbles to safely and temporarily open the BBB in patients with Alzheimer’s disease. The same group also reported the ability of focused ultrasound to open the BBB in areas of the brain afflicted by amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease.
Earlier this year, a team at the West Virginia University Rockefeller Neuroscience Institute reported on the use of focused ultrasound to open the BBB to accelerate the delivery of aducanumab, a treatment for Alzheimer’s disease that was initially approved in 2021.3 This drug has been surrounded by controversy regarding its ability to slow cognitive decline. One issue is that it takes a very long time for the drug to enter the brain due to the BBB, during which time the disease continues to progress. Enter focused ultrasound. The application of this technology could open the BBB and allow for increased delivery of AD drugs to targeted areas of the brain commonly affected by the disease.
The team reported that the temporary opening can last up to 48 hours, allowing increased penetration of aducanumab into the brain. PET scans of trial participants revealed a greater reduction in amyloid plaques in the ultrasound-treated regions of the brain compared to those same regions on the untreated side of the brain. This suggested that more aducanumab was getting into the brain on the treated side. Clearance of plaques was accelerated by 32%, and the amount of plaque was reduced 50% more than in the control areas.4 Although aducanumab has been recently taken off the market due to its questionable efficacy, Dr. Rezai will continue his study with focused ultrasound BBB opening and a different approved drug.
Without a doubt, the use of focused ultrasound will be essential to address some of our most challenging diseases. Focused ultrasound is already changing the way that neurosurgeons are approaching neurodegenerative diseases, and it is advancing rapidly in the field of oncology. This highly versatile technology offers new options for researchers and clinicians as they envision and advance breakthrough therapeutics with the potential to change lives.
References
- Haslam A, Prasad V. Estimation of the percentage of U.S. patients with cancer who are eligible for and respond to checkpoint inhibitor immunotherapy drugs. JAMA Netw. Open. 2019;2:e192535. doi: 10.1001/jamanetworkopen.2019.2535.
- Focused Ultrasound and Cancer Immunotherapy Workshop Summary. Published by the Focused Ultrasound Foundation. https://cdn.fusfoundation.org/2023/11/03164653/FUSF-Cancer-Immunotherapy-Workshop-White-Paper-July-2023.pdf
- Rezai AR, et al. Ultrasound Blood–Brain Barrier Opening and Aducanumab in Alzheimer’s Disease. N Engl J Med 2024; 390:55-62. DOI: 10.1056/NEJMoa2308719
- Rezai A, et al. Ultrasound Blood–Brain Barrier Opening and Aducanumab in Alzheimer’s Disease. N Engl J Med 2024; 390:55-62. DOI: 10.1056/NEJMoa2308719
About The Author:
 Neal Kassell, MD, is the founder and chairman of the Focused Ultrasound Foundation and former co-chair of neurosurgery at the University of Virginia. He has published more than 500 scientific papers and book chapters, and his research has been supported by over $30 million in NIH and industry grants and contracts. A member of numerous medical societies in the U.S. and abroad, he has served on many standing and ad hoc committees of the NIH and in an editorial capacity for a variety of academic journals. In 2016, he was named to the Blue Ribbon Panel of then-Vice President Joe Biden’s Cancer Moonshot Task Force. Kassell is a founder of private ventures including Interax, Inc.; the Virginia Neurological Institute; Multimedia Medical Systems, Inc.; the Neuroclinical Trials Center; the NeuroVenture Fund; and MedSpecialists.net. He has served on corporate and not-for-profit boards, including Eclypsis Corporation; INC Research; the Prostate Cancer Foundation; Insightec, Ltd.; the Expedition Trust Company; Tuesday Evening Concert Series, and Virginia National Bank. Kassell received his undergraduate and medical education at the University of Pennsylvania.
Neal Kassell, MD, is the founder and chairman of the Focused Ultrasound Foundation and former co-chair of neurosurgery at the University of Virginia. He has published more than 500 scientific papers and book chapters, and his research has been supported by over $30 million in NIH and industry grants and contracts. A member of numerous medical societies in the U.S. and abroad, he has served on many standing and ad hoc committees of the NIH and in an editorial capacity for a variety of academic journals. In 2016, he was named to the Blue Ribbon Panel of then-Vice President Joe Biden’s Cancer Moonshot Task Force. Kassell is a founder of private ventures including Interax, Inc.; the Virginia Neurological Institute; Multimedia Medical Systems, Inc.; the Neuroclinical Trials Center; the NeuroVenture Fund; and MedSpecialists.net. He has served on corporate and not-for-profit boards, including Eclypsis Corporation; INC Research; the Prostate Cancer Foundation; Insightec, Ltd.; the Expedition Trust Company; Tuesday Evening Concert Series, and Virginia National Bank. Kassell received his undergraduate and medical education at the University of Pennsylvania.
